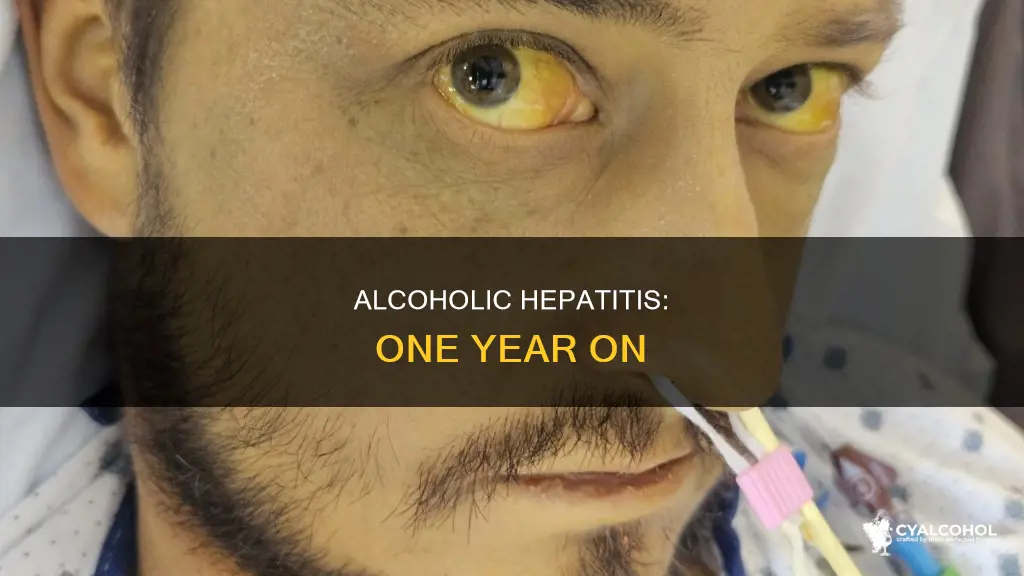
Alcoholic hepatitis is a potentially serious condition caused by alcohol misuse over a long period. It is characterised by jaundice, fever, tachycardia, tachypnea, and hepatomegaly. While heavy drinking over many years can increase the risk of developing alcoholic hepatitis, not everyone who gets it fits this profile. Some people develop alcoholic hepatitis from seemingly insignificant quantities of alcohol, and even shorter durations of alcohol abuse could lead to alcoholic hepatitis. Binge drinking, defined as consuming more than five drinks in a night for men or four for women, at least five times a month is considered heavy drinking and can significantly increase the risk of alcoholic hepatitis within six months.
| Characteristics | Values |
|---|---|
| Definition | Alcoholic hepatitis is an acute inflammation of the liver caused by heavy alcohol consumption. |
| Risk Factors | Heavy drinking over years, genetic differences, family history of alcohol use disorder or liver disease, sex (men can generally tolerate more alcohol). |
| Symptoms | Jaundice, fever, tachycardia, tachypnea, hepatomegaly, leukocytosis with neutrophilia, elevated AST levels, weight loss, abdominal tenderness or soreness, kidney problems, gastrointestinal bleeding, fluid in the belly, confusion, liver cancer, severe infections. |
| Diagnosis | Clinical diagnosis supported by laboratory findings (blood tests, abdominal imaging, liver biopsy). |
| Treatment | Stopping alcohol consumption, dietary changes (low-sodium, vitamin supplements), antibiotics, corticosteroids, liver transplant (in severe cases). |
| Prognosis | If alcohol consumption continues after diagnosis, reduced life expectancy. Severe cases can lead to cirrhosis, liver failure, and death. |
| Prevention | Reducing or stopping alcohol intake, adhering to recommended drinking limits. |
What You'll Learn

Binge drinking and heavy alcohol consumption
The risks associated with binge drinking are not limited to immediate harms but also extend to long-term health problems. Chronic heavy drinking over years can cause significant liver damage and increase the risk of developing alcoholic hepatitis, cirrhosis, and other types of liver disease. It is important to note that the progression to alcohol-induced liver disease is not solely dependent on the amount of alcohol consumed, and even shorter durations of alcohol abuse or seemingly insignificant quantities can lead to alcoholic hepatitis in some individuals.
Excessive alcohol consumption is a leading preventable cause of death. It increases the risk of several types of cancer, heart disease, high blood pressure, digestive problems, mental health conditions, and learning difficulties. Additionally, heavy drinking can negatively impact relationships, cause financial challenges, and lead to social and ethical concerns. It is essential to recognise that alcohol use disorder (AUD) affects a significant proportion of individuals, and seeking professional help is crucial for managing harmful drinking behaviours.
The good news is that quitting alcohol after a diagnosis of alcoholic hepatitis can lead to significant improvement within six to 12 months, and milder cases often resolve completely. Abstaining from alcohol can prevent further liver damage and help individuals recover, even if some permanent scarring remains. However, continuing to drink after diagnosis leads to a reduced life expectancy, with poorer outcomes for those with severe alcohol-induced hepatitis and advanced liver disease.
Alcohol Tolerance: Can It Lower?
You may want to see also

Risk factors and individual differences
While heavy drinking over many years is a significant risk factor for alcoholic hepatitis, it is important to note that not everyone who consumes large amounts of alcohol will develop this disease. Individual factors, such as genetic differences, sex, and sensitivity to alcohol, also play a role in the development of alcoholic hepatitis.
Genetics and family history can influence an individual's risk for alcoholic hepatitis. Research suggests that some people are more sensitive to alcohol, and their livers react to even moderate use. If an individual has a family history of alcohol use disorder or liver disease, their risk for alcoholic hepatitis may be higher.
Sex differences also contribute to the development of alcoholic hepatitis. Generally, men can tolerate more alcohol than women. For example, heavy drinking is defined as consuming more than five drinks in a night for men or four for women. However, it is important to note that everyone is different, and there is no universally "safe" amount of alcohol that guarantees protection from alcoholic hepatitis.
The amount of alcohol ingested is the most important risk factor for alcoholic hepatitis. Binge drinking, defined as consuming more than four to five drinks in a night, at least five times a month, is considered heavy drinking. Maintaining this pace for at least six months significantly increases the risk of developing alcoholic hepatitis. However, it is important to note that even shorter durations of alcohol abuse could lead to alcoholic hepatitis.
In addition to the quantity of alcohol consumed, the progression to alcohol-induced chronic liver disease is influenced by individual differences in the body's response to alcohol. The correlation between the amount of alcohol consumed and liver injury is not linear, and some people develop alcoholic hepatitis from seemingly insignificant quantities of alcohol.
While the exact mechanisms are not yet fully understood, it is clear that individual differences play a significant role in the development of alcoholic hepatitis. Further research is necessary to confirm why some people who drink in excess develop the disease while others do not.
Alcohol: Limit or Quit?
You may want to see also

Diagnosis and treatment options
Alcoholic hepatitis (AH) is typically diagnosed based on a patient's history of heavy alcohol consumption, recent onset of jaundice, and exclusion of other causes of acute liver injury. Laboratory findings, such as elevated AST levels and typical biochemical patterns, also support the diagnosis. Ultrasound is often used as the first imaging test to assess the liver and exclude gallstones or other biliary tract disorders. While not always necessary, a liver biopsy can be useful for excluding other disorders, but it should be performed with caution due to the patient's potential coagulopathy and thrombocytopenia.
In terms of treatment, the most critical step is abstinence from alcohol. If patients quit drinking completely and permanently, their condition can improve significantly within six to twelve months, and they can even recover fully in milder cases. However, continuing to drink alcohol will lead to further liver damage and cirrhosis.
For severe cases of AH, healthcare providers may prescribe steroids to reduce inflammation and encourage liver cell regeneration. Liver transplantation is another treatment option for patients who do not respond to steroids, although this approach faces barriers such as organ shortage and ethical considerations. A study found that prednisolone therapy provided a borderline reduction in mortality for patients with AH during the first 28 days of treatment but showed no benefit after 90 days or one year.
Cutting Down or Quitting Alcohol: Which is Better?
You may want to see also

Reversing alcoholic hepatitis
Alcoholic hepatitis is a syndrome of jaundice and liver failure that occurs in heavy consumers of alcohol. It is caused by heavy drinking over years, though shorter durations of alcohol abuse could also lead to alcoholic hepatitis. Binge drinking, defined as more than five drinks in a night for men or four for women, at least five times a month is considered heavy drinking.
The treatment for alcoholic hepatitis often depends on whether the patient is willing to stop drinking alcohol and make changes to their lifestyle. Abstaining from alcohol is essential for long-term survival. If the condition is not too far advanced, it can be reversed by quitting alcohol. People who quit drinking alcohol after diagnosis show great improvement after six to 12 months. Milder cases often resolve completely, while more severe cases can continue to show gradual improvement over the following years. However, existing scar tissue in the liver cannot be reversed, but further damage can be prevented and the rest of the liver preserved by quitting alcohol.
In severe cases of alcoholic hepatitis, hospital treatment may be necessary. Specific treatment with corticosteroids or pentoxifylline may be used to reduce inflammation of the liver. Nutritional support is also an important part of treatment in these cases. Liver transplantation is currently the only way to cure irreversible liver failure.
Psychological therapy and self-help groups such as Alcoholics Anonymous can be useful in helping patients stop drinking. Additionally, malnutrition is common in people with alcoholic hepatitis, so eating a balanced diet is important to ensure patients get all the nutrients they need.
Why Alcohol Groups Are More Polar Than Carbonyl Groups
You may want to see also

Liver transplantation considerations
While it is unclear whether alcoholic hepatitis can develop in one year, heavy drinking over many years is a common cause of alcoholic hepatitis. Binge drinking, defined as more than five drinks in a night for men or four for women, at least five times a month, is considered heavy drinking. Even shorter durations of alcohol abuse could lead to alcoholic hepatitis, as some people are more sensitive to alcohol and their livers react to even moderate use.
Patient Selection
The selection process for liver transplantation candidates involves multiple medical teams, the patient's family, and the patient. The patient's commitment to lifelong total alcohol abstinence is crucial, and they must be supported by their family members. The patient should also not have any severe coexisting conditions or psychiatric disorders.
Medical Therapy
Medical therapy for alcoholic hepatitis typically includes standard medical care for severe liver insufficiency and the use of glucocorticoids (e.g., 40 mg per day of prednisolone for at least 7 days). Non-response to medical therapy is defined by the Lille model as a score of 0.45 or higher after 7 days, indicating an increased risk of death and non-response to therapy.
Timing of Transplantation
The timing of liver transplantation for alcoholic hepatitis is a critical consideration. Early liver transplantation can improve survival in patients with severe alcoholic hepatitis not responding to medical therapy. However, there is a reluctance to perform transplantation due to concerns about the limited organ supply and the risk of relapse into harmful drinking. Most transplant centres require a minimum of six months of abstinence from alcohol before considering transplantation, but this rule has been controversial.
Graft Rejection and Relapse
Graft rejection and relapse rates are important considerations in liver transplantation for alcoholic hepatitis. Retrospective studies have shown that graft rejection rates were higher among abstinent patients, while relapse rates were similar between patients with and without alcoholic hepatitis.
Centre Protocols
Liver transplant centres should establish formal protocols to guide patient selection and post-transplant follow-up. Creating standardised criteria for patient selection can help ensure equitable access to liver transplantation for eligible candidates with alcoholic hepatitis.
Alcohol and Surgery: A Dangerous Mix?
You may want to see also
Frequently asked questions
Yes, alcoholic hepatitis can develop in less than a year, especially if one engages in binge drinking, which is considered five or more standard drinks within a few hours for men and four for women, at least five times a month. However, it typically develops over many years of heavy drinking.
Symptoms of alcoholic hepatitis include jaundice, fever, stomach ache, weight loss, and liquid buildup in the belly. Some people with mild hepatitis may not experience any symptoms.
The most critical part of treating alcoholic hepatitis is stopping alcohol consumption. Other treatments include medications, therapy, support groups, dietary changes, antibiotics, and steroids. In severe cases, a liver transplant may be required.