Alcohol withdrawal syndrome and alcohol withdrawal are related, but they are not the same. Alcohol withdrawal is a set of symptoms that can develop when a person who has been drinking heavily on a regular basis suddenly stops or significantly reduces their alcohol intake. Alcohol Withdrawal Syndrome (AWS) is a more severe form of alcohol withdrawal, characterised by more severe symptoms such as seizures and delirium tremens. To be diagnosed with AWS, patients must exhibit at least two of the following symptoms: increased hand tremor, insomnia, nausea or vomiting, transient hallucinations, psychomotor agitation, anxiety, generalised tonic-clonic seizures, and autonomic instability. While most people who go through alcohol withdrawal make a full recovery, it can be a serious, life-threatening condition.
| Characteristics | Values |
|---|---|
| Definition | Alcohol withdrawal syndrome refers to a set of symptoms that can develop if you stop or significantly reduce alcohol intake after long-term use. |
| Diagnosis | Healthcare providers make a diagnosis of alcohol withdrawal syndrome based on a physical exam, symptoms, alcohol use history, and medical history. |
| Symptoms | Symptoms range from mild (e.g., insomnia, tremors, anxiety) to severe and life-threatening (e.g., hallucinations, delirium tremens, seizures) |
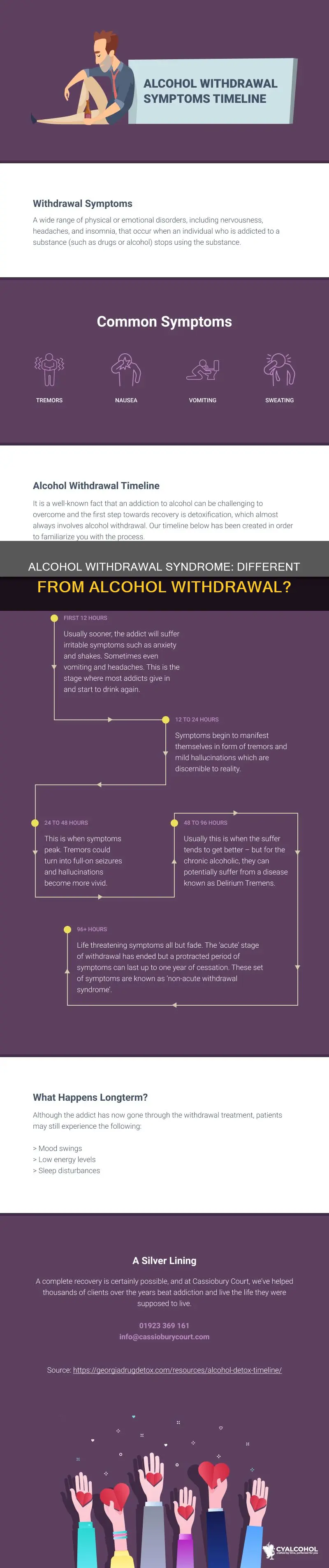
| Onset | Symptoms typically begin 6-24 hours after the last drink, peak at 24-72 hours, and can last for several days or weeks. |
| Treatment | Treatment options include inpatient and outpatient settings, with medications such as benzodiazepines and carbamazepine commonly used to manage symptoms. |
| Prognosis | Most people who go through alcohol withdrawal make a full recovery, but death is possible, especially with severe complications. |
| Prevention | Total and lifelong avoidance of alcohol (abstinence) is recommended to prevent alcohol withdrawal syndrome. |
What You'll Learn

Alcohol withdrawal symptoms
Psychologically, you may experience rapid changes in mood, which can range from mild to serious and can sometimes be life-threatening. About 12-48 hours after you stop drinking, more serious symptoms can start, including hallucinations and seizures. Delirium tremens (DTs) is a severe form of alcohol withdrawal that can cause fatal complications. Symptoms of DTs include repeated vomiting, severe shaking, and hallucinations. If you experience seizures, you should seek medical help immediately, as they can result in permanent injury or death.
The severity and duration of alcohol withdrawal symptoms vary depending on individual factors, such as the amount of alcohol typically consumed and the duration of alcohol use. Symptoms tend to occur within eight hours after the last drink but can also appear days later. They typically peak within 24 to 72 hours but may persist for weeks or even months.
If you are experiencing alcohol withdrawal symptoms, it is important to seek medical support to help you reduce and stop your alcohol consumption safely. Treatment options include specific prescription medications and supportive environments to manage mild to moderate symptoms. In more severe cases, hospitalisation may be necessary to closely monitor vital signs and prevent complications.
Alcohol Rules at Walker County Public Lake, Alabama
You may want to see also

Diagnosis and treatment
Alcohol withdrawal syndrome (AWS) is a set of symptoms that can develop if a person stops or significantly reduces their alcohol intake after long-term use. AWS can range from mild to severe. Mild symptoms include anxiety, headaches, gastrointestinal discomfort, and insomnia. These symptoms can progress to severe manifestations, such as alcohol withdrawal delirium (DTs), which can be life-threatening.
Diagnosis of AWS is typically made by a healthcare provider based on a physical exam, the patient's symptoms, alcohol use history, and medical history. It is important for the patient to be honest about their alcohol use and any other substance use to receive the best care. The provider may also recommend additional tests, such as blood tests, urine tests, and an EKG (electrocardiogram), to check the patient's overall health and assess for conditions such as dehydration, electrolyte imbalances, liver function issues, heart issues, and gastrointestinal bleeding.
Treatment for AWS varies depending on the severity of symptoms. Mild cases may only require a supportive environment, while moderate cases may need short-term medications to lessen symptoms. In severe cases, hospitalization or treatment in a specialized facility may be necessary to monitor for hallucinations and other signs of delirium tremens (DTs). Benzodiazepines are often used to reduce the risk of progression to severe AWS, and patients should also receive thiamine and folate supplementation due to their high risk of nutritional deficiencies.
It is important for patients experiencing AWS to seek medical help and to have someone monitor their symptoms, as alcohol withdrawal can be unpredictable and potentially life-threatening. Outpatient settings may be suitable for mild-to-moderate cases, while more severe cases may require treatment in an emergency room, intensive care unit, or detoxification facility. Total and lifelong avoidance of alcohol (abstinence) is recommended for individuals who have gone through AWS to prevent relapse and future health complications.
Various resources are available to individuals experiencing AWS, including hotlines such as SAMHSA's National Helpline, which offers free, confidential referrals to local treatment facilities, support groups, and community-based organizations. It is important to seek help and support during AWS to ensure the best chances of recovery and to prevent severe complications.
Alcohol Sales on Labor Day in New Mexico
You may want to see also

Alcohol withdrawal delirium
AWD is characterised by profound global confusion, agitation, disorientation, hallucinations, fever, hypertension, diaphoresis, and autonomic hyperactivity (tachycardia and hypertension), which can progress to cardiovascular collapse. It is caused by excessive nervous system excitability during periods of abstinence from alcohol. When alcohol is withdrawn, the brain's neurotransmitters are no longer suppressed, but because they are used to working harder to overcome the suppression, they go into a state of overexcitement. This overexcitement can lead to severe confusion, anxiety, seizures, and delirium.
AWD typically sets in 48 to 72 hours after the last drink, with most symptoms peaking five days after they begin and decreasing about five to seven days later. However, symptoms can start as early as two hours after the last drink, and it is most likely to begin between six hours to a day after the last drink. The risk of developing AWD increases with the frequency and quantity of alcohol consumption. According to the U.S. National Institute on Alcohol Abuse and Alcoholism (NIAAA), heavy drinking is defined as consuming five or more drinks on any day or 15 or more per week for male adults and four or more drinks on any day or eight or more drinks per week for female adults.
The treatment of AWD includes providing a calm, quiet, well-lit environment, reassurance, ongoing reassessment, attention to fluid and electrolyte deficits, and treatment of any coexisting addictions. Various medications can be used in the treatment and supportive care of AWD, including benzodiazepines (such as chlordiazepoxide, diazepam, and lorazepam) and anesthetic agents (such as propofol, dexmedetomidine, and ketamine). Thiamine can also be useful for preventing Wernicke encephalopathy and Korsakoff syndrome, which are disorders caused by thiamine deficiency.
Is Alcohol Safe for Sanded Drywall?
You may want to see also

Protracted alcohol withdrawal syndrome
Alcohol withdrawal refers to symptoms that may occur when a person who has been drinking too much alcohol regularly suddenly stops drinking or significantly reduces their alcohol intake. Alcohol withdrawal symptoms can range from mild to severe and may last for months.
Protracted alcohol withdrawal can be characterized by symptoms such as anxiety, hostility, irritability, depression, mood changes, fatigue, insomnia, problems with concentration and thinking, decreased sex drive, and unexplained physical pain. Sleep studies suggest that sleep problems can persist for 1-3 years after alcohol consumption stops. It is important to note that these symptoms can ebb and flow, and they tend to subside with continued abstinence.
The diagnosis of protracted withdrawal is not included in the "Diagnostic and Statistical Manual of Mental Disorders" due to a lack of consensus on the syndrome's definition and treatment. However, chronic alcohol use can lead to changes in the brain's molecular, cellular, and neurocircuitry, affecting emotions and behaviors even after acute withdrawal symptoms have ended.
If you or someone you know is experiencing symptoms of alcohol withdrawal, it is important to seek medical help. Treatment options for alcohol withdrawal may include hospitalization or outpatient care, depending on the severity of symptoms. Lifelong abstinence from alcohol is the safest approach to prevent further complications.
Alcohol Laws on Montana Reservations: Explained
You may want to see also

Alcohol withdrawal seizures
Alcohol is a central nervous system depressant, slowing down brain function and altering nerve communication. With prolonged alcohol exposure, the body develops tolerance and physical dependence, resulting in compensatory changes in the brain's ion channels and neurotransmitter receptors. Abruptly stopping alcohol consumption unmasks these changes, leading to withdrawal symptoms, including seizures.
Generalized tonic-clonic seizures are the most common and severe type of alcohol withdrawal seizures, characterised by muscular rigidity and convulsions. These seizures are triggered by neuronal networks in the brainstem, particularly the inferior colliculus, and are distinct from other types of seizures due to their pharmacological induction.
The risk of alcohol withdrawal seizures can be reduced by gradually tapering alcohol intake under medical supervision. For moderate alcohol withdrawal, benzodiazepines or barbiturates are often prescribed to prevent seizures and delirium tremens. Severe cases may require hospitalisation, continuous monitoring, and additional treatments for related health issues such as dehydration and electrolyte imbalances.
It is crucial to seek medical assistance during alcohol withdrawal to ensure proper management and prevent potentially life-threatening complications.
Alcohol at Be Our Guest: Lunchtime Libations
You may want to see also
Frequently asked questions
Alcohol withdrawal is a set of symptoms that can develop if you stop or significantly reduce alcohol intake after long-term use. Symptoms can range from mild to severe and can include sleep changes, rapid changes in mood, and fatigue.
Alcohol withdrawal syndrome is a condition where patients exhibit at least two symptoms of alcohol withdrawal, including insomnia, trembling, nausea or vomiting, transient hallucinations, psychomotor agitation, anxiety, and autonomic instability. The condition can be diagnosed through a physical exam, the patient's symptoms, alcohol use history, and medical history.
Alcohol withdrawal is an umbrella term for the symptoms that occur when one stops drinking alcohol. Alcohol withdrawal syndrome is a specific diagnosis given to patients exhibiting at least two symptoms of alcohol withdrawal.