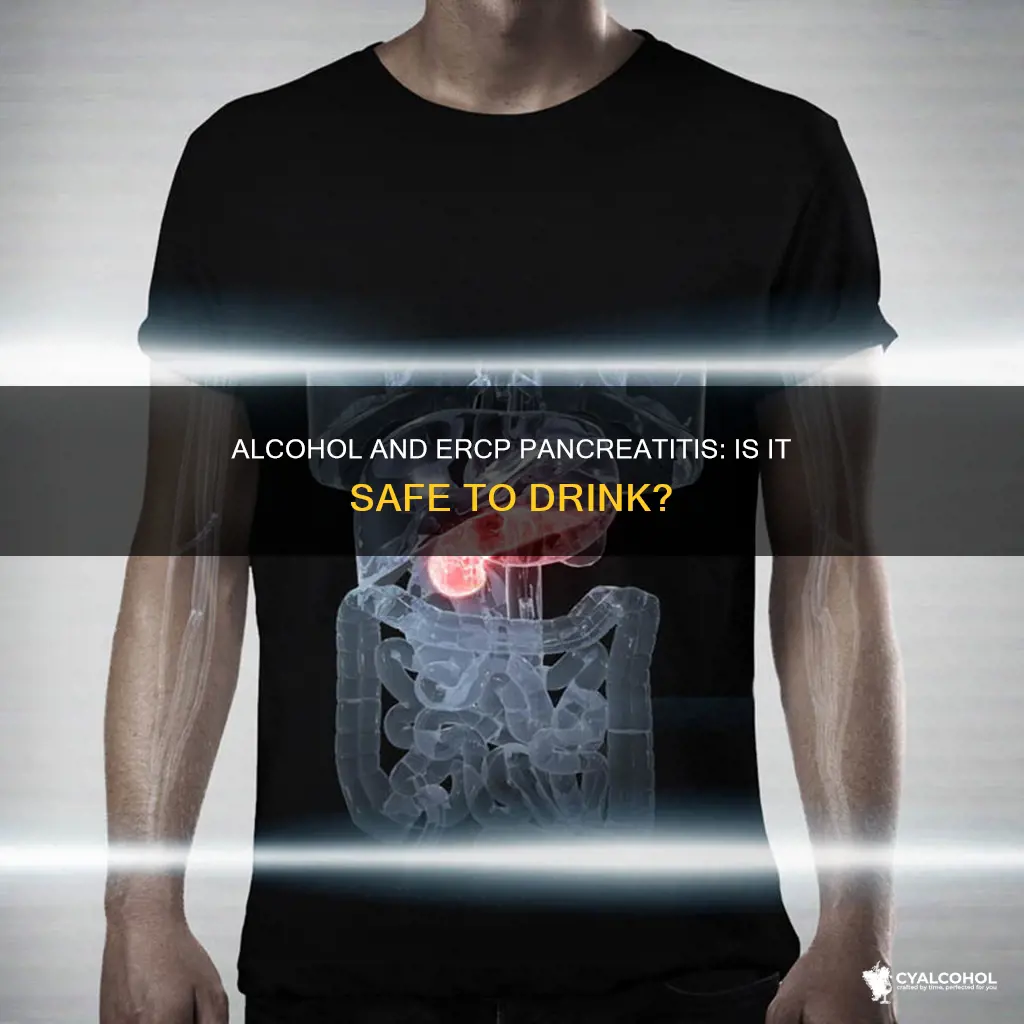
Alcohol consumption is a leading cause of acute pancreatitis, with heavy drinking increasing the risk of repeated episodes. Alcohol abuse can lead to permanent damage to the pancreas, resulting in chronic pancreatitis. While the relationship between alcohol consumption and ERCP pancreatitis is not yet fully understood, studies have shown that current alcohol use is a significant predictor of ERCP pancreatitis. Therefore, it is generally recommended to abstain from alcohol after an episode of acute pancreatitis to prevent further damage to the pancreas and reduce the risk of recurrence. However, the decision to consume alcohol after pancreatitis should be made in consultation with a healthcare professional, considering individual health factors and lifestyle.
| Characteristics | Values |
|---|---|
| Should I consume alcohol if I had ERCP pancreatitis? | There is no clear answer, but it is generally advised to avoid alcohol after an episode of acute pancreatitis. |
| Factors to consider | Severity of pancreatitis, its cause, individual health profile, lifestyle factors, and doctor's advice. |
| Risks of alcohol consumption after pancreatitis | Increased risk of recurrence, potentially more severe episodes, permanent damage to the pancreas, and severe abdominal pain. |
| Alcohol-related pancreatitis | Alcohol is a leading cause of acute and chronic pancreatitis, with heavy drinking increasing the risk. |
| Prevention and management | Completely stopping alcohol prevents further alcohol-related damage to the pancreas. |
| Smoking | Cigarette smoking is also a risk factor for pancreatitis and can accelerate disease progression. |
What You'll Learn
- Alcohol is a leading cause of acute pancreatitis
- Alcohol consumption can cause permanent damage to the pancreas
- The risks associated with drinking alcohol after acute pancreatitis are significant
- The amount and duration of alcohol consumption are the most important determinants of the risk of pancreatitis
- Abstaining from alcohol after acute pancreatitis is the safest choice

Alcohol is a leading cause of acute pancreatitis
Alcohol consumption is linked to 21.3% of deaths from digestive diseases, with pancreatitis and liver cirrhosis being the most common. Alcohol is broken down into substances that are toxic to the pancreas, and heavy drinking over a long period can cause acute pancreatitis. The risk increases with the number of drinks consumed, and drinking patterns have been shown to be considerably high in patients diagnosed with acute pancreatitis. One study found that patients consumed, on average, 7-10 drinks per drinking day.
The type of alcohol consumed also influences the risk. Hard liquor is associated with a higher risk of triggering acute pancreatitis compared to beer or wine. However, this does not mean that beer or wine is safe, only that they are less risky. The amount consumed is a more important factor than the type of alcohol.
Alcohol-induced pancreatitis occurs due to prolonged, chronic alcohol use. It causes the pancreatic tissue to autodigest and leads to further inflammation. Additionally, alcohol use can cause premature activation of trypsinogen and other digestive enzymes within the acinar cells, resulting in up to 50% of pancreatic tissue damage.
The decision to consume alcohol after acute pancreatitis should be made with medical advice. Even moderate drinking can be harmful to a recovering pancreas, and the risks associated with alcohol consumption following an acute pancreatitis episode are significant.
Reckless Driving in Delaware: Alcohol and the Law
You may want to see also

Alcohol consumption can cause permanent damage to the pancreas
The association between alcohol abuse and pancreatic injury has been recognised since 1878. Alcohol consumption can lead to pancreatitis due to the toxic effects of its metabolites, such as acetaldehyde and fatty acid ethyl esters, and the by-products of ethanol metabolism, such as reactive oxygen species. Alcohol metabolism can also lead to oxidant stress within the pancreas, causing damage to acinar cells, ductal cells, and stellate cells, which can result in acinar cell death, calcification, and fibrosis.
Additionally, alcohol can cause premature activation of digestive enzymes in the pancreas, leading to autodigestion of the pancreas and further damage. This process is supported by evidence of increased synthesis of digestive enzymes in the pancreas following alcohol consumption. Furthermore, alcohol decreases the stability of zymogen granules and lysosomes, which contain digestive and lysosomal enzymes, respectively. The accumulation of these enzymes within the cells can have detrimental effects.
It is important to note that even if an individual was not a heavy drinker before experiencing pancreatitis, alcohol can still be harmful to a recovering pancreas. Continuing to drink alcohol after acute pancreatitis can increase the risk of recurrence and lead to more severe episodes. Therefore, it is generally recommended to abstain from alcohol after an episode of acute pancreatitis to prioritise health and quality of life.
Dye Na Flow vs Alcohol Ink: What's the Difference?
You may want to see also

The risks associated with drinking alcohol after acute pancreatitis are significant
Heavy drinking can lead to repeated episodes of acute pancreatitis, which can permanently damage the pancreas and lead to chronic pancreatitis. Even if alcohol was not the root cause of the initial acute pancreatitis, the risks associated with alcohol consumption following an acute pancreatitis episode are significant and should be carefully considered. The severity of pancreatitis, its cause, and individual health profiles play crucial roles in determining one's long-term relationship with alcohol.
If pancreatic function has not completely returned to normal, the risks of alcohol consumption are likely heightened. Even if one was not a heavy drinker before their pancreatitis, alcohol can still be harmful to a recovering pancreas. The goal after pancreatitis should not be to return to previous drinking habits. If alcohol is reintroduced, it should be at minimal levels and only with a doctor's explicit approval.
It is important to note that what may be considered moderate drinking for one person may be excessive for another, especially someone with a history of pancreatitis. This is not a time to test limits, and following a doctor's precise instructions is crucial. The decision to consume alcohol after acute pancreatitis should be made in consultation with a healthcare team, weighing the potential benefits of alcohol enjoyment against the significant risks to health and well-being. Ultimately, for many, the safest choice is to abstain from alcohol completely following an episode of acute pancreatitis.
Carrying Concealed Weapons and Alcohol: A Legal Mix?
You may want to see also

The amount and duration of alcohol consumption are the most important determinants of the risk of pancreatitis
While the type of alcoholic beverage may influence the risk of pancreatitis, the amount and duration of alcohol consumption are considered the most crucial factors in determining the likelihood of developing the disease. The role of beverage type requires further investigation, but it is widely accepted that the amount of alcohol consumed has a more significant impact on the risk of pancreatitis than the type of drink.
Heavy alcohol consumption is associated with acute and recurrent pancreatitis, a painful and potentially fatal inflammatory condition that can cause severe abdominal pain. The condition can lead to nausea, vomiting, and other complications. It is believed that alcohol consumption, in combination with other factors, increases the vulnerability of the pancreas to inflammation. As the pancreas breaks down alcohol, it produces substances that are toxic to the organ, and over time, this can result in pancreatitis.
The risk of developing pancreatitis increases with the number of drinks consumed. While the threshold for safe consumption is unclear, drinking two or more alcoholic beverages daily can significantly increase the risk. Binge drinking and regular drinking patterns may also be important factors in increasing the likelihood of pancreatitis. Additionally, the risk of pancreatitis varies between individuals and can be influenced by factors such as smoking, hypertriglyceridemia, and genetic factors.
For individuals who have experienced alcohol-related pancreatitis or recurrent acute or chronic pancreatitis, even small amounts of alcohol consumption can lead to disease progression. Therefore, it is generally recommended to abstain from alcohol after an episode of acute pancreatitis, as the risks associated with alcohol consumption are significant. Continuing to drink alcohol after acute pancreatitis can increase the risk of recurrence and progression to chronic pancreatitis.
It is important to note that the decision to consume alcohol after acute pancreatitis should be made in consultation with a healthcare professional, who can provide precise instructions based on an individual's health profile, the severity of pancreatitis, and its underlying causes.
Alcohol Overdose: Difficulty Breathing a Warning Sign?
You may want to see also

Abstaining from alcohol after acute pancreatitis is the safest choice
Acute pancreatitis is a sudden inflammation of the pancreas, a vital organ responsible for producing enzymes that aid in digestion and hormones like insulin to regulate blood sugar. This inflammation can cause severe abdominal pain, nausea, and vomiting, among other complications. While gallstones are a significant cause, alcohol abuse is another leading culprit.
Alcohol consumption is a significant risk factor for acute pancreatitis, and heavy drinking can lead to repeated episodes, increasing the severity of the condition. Even if alcohol was not the root cause of the initial episode, continuing to consume alcohol after recovering from acute pancreatitis can make a future episode more likely and more severe. Therefore, it is crucial to consider the risks associated with alcohol consumption following an acute pancreatitis episode.
The decision to consume alcohol after acute pancreatitis should be made in consultation with a healthcare professional, as the potential benefits of alcohol enjoyment must be weighed against the significant risks to health and well-being. It is important to remember that an individual's health and quality of life should always be the priority. For many people, the safest and most responsible choice is to abstain from alcohol completely following an episode of acute pancreatitis.
While a complete lifetime ban on alcohol may not be necessary for everyone, the risks associated with alcohol consumption after acute pancreatitis are significant. The severity of pancreatitis, its cause, and individual health factors play crucial roles in determining one's long-term relationship with alcohol. Even if one was not a heavy drinker before pancreatitis, alcohol can still be harmful to a recovering pancreas. Therefore, if alcohol is reintroduced, it should be at minimal levels and only with a doctor's explicit approval.
Additionally, it is important to address other lifestyle factors, such as smoking, which is also associated with an increased risk of acute pancreatitis. By quitting smoking and abstaining from alcohol, individuals can significantly reduce their risk of future episodes of acute pancreatitis and improve their overall health and well-being.
How Evaporation Transforms Alcohol: Chemistry or Physics?
You may want to see also
Frequently asked questions
There is limited research on the relationship between alcohol consumption and ERCP pancreatitis. However, current alcohol consumption is considered a new risk factor for PEP. It is best to consult your healthcare team and follow their precise instructions.
ERCP stands for endoscopic retrograde cholangiopancreatography. It is a procedure that involves inserting a flexible tube into the mouth and advancing it to the small intestine to treat pancreatic diseases.
Apart from current alcohol consumption, other risk factors for ERCP pancreatitis include former cigarette smoking, suspected sphincter of Oddi dysfunction (SOD), pancreatic sphincterotomy, and moderate/difficult cannulation.