Delirium tremens (DTs) is a severe form of alcohol withdrawal that can be life-threatening. It occurs when someone with alcohol use disorder, particularly moderate to severe cases, abruptly stops drinking. The symptoms of DTs can be dangerous and include confusion, tremors, agitation, psychosis, seizures, and hallucinations. Given the severity of these symptoms, it is recommended that individuals experiencing DTs seek immediate medical attention and hospitalization. Treatment for DTs focuses on stabilizing the patient, relieving symptoms, and preventing complications, often through the use of sedatives and intravenous fluids. Long-term preventive treatment aims for total alcohol abstinence and may involve support groups and therapy.
| Characteristics | Values |
|---|---|
| Should you go to the hospital? | Yes, a hospital stay is needed. |
| Treatment | Alcohol rehabilitation, antipsychotic drugs, sedatives, intravenous fluids, vitamins, minerals, CBT, recovery support groups, detox, inpatient/residential care, intensive outpatient programs, partial hospitalization programs, outpatient care, aftercare, sober living solutions |
| Symptoms | Confusion, tremors, agitation, anxiety, psychosis, hallucinations, paranoia, sensory disruptions, disorientation, heavy sweating, seizures, heart attack, stroke, death, nightmares, high heart rate, high blood pressure, fever, shaking, shivering, irregular heart rate, tactile hallucinations, visual hallucinations, auditory hallucinations |
| Underlying issues | Alcohol use disorder, moderate or severe alcohol use disorder, heavy drinking, frequent alcohol use, withdrawal, history of mental health issues, depression, post-traumatic stress disorder, bipolar disorder, dementia, heart disease, head injury, infection, illness, poor general health, lack of well-balanced diet, electrolyte abnormalities, pancreatitis, alcoholic hepatitis |
| Prevention | Lower alcohol use, alcohol abstinence, screening tools, treatment for alcohol dependence |
What You'll Learn

Alcohol withdrawal symptoms
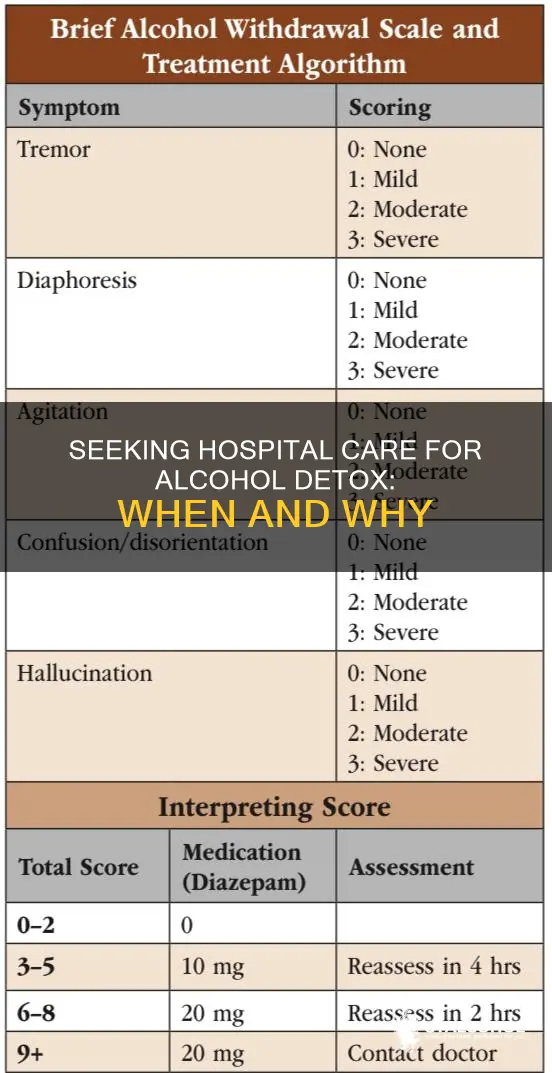
The symptoms of alcohol withdrawal can be both physical and psychological. Mild symptoms may include agitation, anxiety, insomnia, tremors, heavy sweating, and confusion. More severe symptoms can include hallucinations (seeing, hearing, or feeling things that aren't real), seizures, and delirium tremens (DTs). DTs is the most severe form of alcohol withdrawal and can be life-threatening. It is characterised by symptoms such as confusion, agitation, psychosis (including hallucinations and paranoia), sensory disruptions, disorientation, heavy sweating, and seizures. DTs usually occur within 2 to 5 days of the last alcohol consumption and can last for several days, with symptoms peaking in intensity around this time.
It is important to recognise the danger signs of alcohol withdrawal and seek medical attention if necessary. If someone is experiencing severe symptoms such as repeated vomiting, severe shaking, hallucinations, or seizures, they should seek immediate medical help. Alcohol withdrawal can be managed and treated under proper medical supervision. Treatment for alcohol withdrawal aims to relieve symptoms, reduce complications, and save lives if necessary. Treatment options can include medications such as sedatives (typically benzodiazepines) to calm the nervous system, antipsychotic drugs to prevent hallucinations, and in some cases, anaesthesia to induce complete sedation until symptoms subside. Intravenous fluids, vitamins, and minerals may also be administered to treat dehydration and electrolyte imbalances.
In addition to medical treatment, it is crucial to address the underlying issue of alcohol use disorder. This may involve detoxification, rehabilitation, and ongoing support through cognitive-behavioural therapy (CBT), recovery support groups, or other treatment plans. Seeking professional help is essential to safely manage alcohol withdrawal and to develop a long-term plan for recovery and relapse prevention.
Michigan Alcohol Taxes: What's the Deal?
You may want to see also

Treatment options
Hospitalization
Delirium tremens is a medical emergency and often requires immediate treatment in a hospital or admission to a dedicated detox centre. Inpatient care allows for continuous monitoring of vital signs, fluid balance and mental status to address any complications in real time. If symptoms cannot be managed with sedatives, complete sedation may be induced with anaesthesia until symptoms end.
Medication
A combination of medications is typically used to manage DTs, often administered in a hospital setting. Benzodiazepines are the cornerstone of DT treatment, helping to calm the overactive nervous system, reduce agitation and lower the risk of seizures. They include medications such as diazepam (Valium), chlordiazepoxide (Librium) or lorazepam (Ativan).
Antipsychotics are also used to manage psychosis and severe or ongoing hallucinations. Drugs like haloperidol (Haldol) may be prescribed to help manage these symptoms.
Fluid and Electrolyte Support
IV fluids, vitamins (especially thiamine) and electrolytes help restore balance and counteract dehydration or malnutrition.
Nutritional Support
Reintroducing a balanced diet, vitamins and supplements helps to stabilize health. Many individuals with severe alcohol use disorder also struggle with poor nutrition.
Psychological Support
DTs can be terrifying, so ongoing recovery resources, such as therapy, 12-step programmes or outpatient treatment can reduce the risk of relapse and the subsequent danger of repeated withdrawal episodes. Cognitive behavioural therapy (CBT) or recovery support groups, such as Alcoholics Anonymous, may help maintain sobriety moving forward.
Prevention
If you are dependent on alcohol and considering stopping, it’s best to seek medical advice rather than attempting to detox alone. This can include aftercare and support, such as therapy, 12-step programmes or outpatient treatment.
Alcohol in Cars: Is it Legal?
You may want to see also

Underlying health issues
Delirium tremens (DTs) is a severe form of alcohol withdrawal that can be life-threatening and requires immediate medical attention. It is characterized by both physical and psychological symptoms, including hallucinations, agitation, tremors, rapid heartbeat, high blood pressure, fever, and sweating.
Addressing underlying health issues is a crucial aspect of managing DTs and preventing future occurrences. Here are some key considerations regarding underlying health issues in the context of DTs:
Co-occurring Medical Conditions: DTs often co-exist with other medical conditions that require attention. These can include cardiovascular disease, liver disease, nutritional deficiencies (such as Wernicke-Korsakoff syndrome), electrolyte imbalances, mineral deficiencies, and other health complications. Treating these co-morbidities is an essential component of comprehensive DTs management.
Mental Health Disorders: Mental health issues are commonly associated with DTs. Individuals with a history of mental health disorders, such as depression, post-traumatic stress disorder, bipolar disorder, or other psychiatric conditions, are at an increased risk of experiencing DTs. Addressing these underlying mental health concerns is vital for successful recovery. This may include cognitive behavioral therapy (CBT), individual or group therapy, addiction counselling, support groups, and family therapy.
Age and Health Status: Advancing age is a risk factor for developing DTs. Older individuals are more susceptible to experiencing DTs and may also have additional physical health conditions that complicate the management of DTs. Poor general health, including a lack of a well-balanced diet, can further exacerbate the risks associated with DTs. Therefore, addressing nutritional deficiencies and improving overall health can help mitigate the impact of underlying health issues on DTs.
Alcohol Use Disorder: While not strictly an underlying health issue, alcohol use disorder is the primary driver of DTs. Addressing this disorder through treatment and rehabilitation is essential to prevent relapses and future occurrences of DTs. This may involve behavioural treatment, medication, support groups, and lifestyle changes to reduce alcohol consumption and manage triggers.
Previous Withdrawal Symptoms: Experiencing severe alcohol withdrawal symptoms previously, including DTs or withdrawal seizures, is a risk factor for developing DTs again. Therefore, addressing underlying health issues that may have contributed to previous withdrawal symptoms is crucial for preventing DTs in the future.
Alcohol and Type 2 Diabetes: Exploring the Link
You may want to see also

Preventative measures
Delirium tremens (DTs) is a severe and life-threatening form of alcohol withdrawal. It is a medical emergency that requires immediate treatment and inpatient care. DTs usually occur when someone with alcohol use disorder suddenly stops drinking. Therefore, it is recommended to consult a doctor before stopping alcohol consumption.
- Alcohol Rehabilitation Care: Seeking professional help through alcohol rehabilitation programmes can help individuals lower their alcohol intake or stop drinking entirely, reducing the risk of developing DTs.
- Gradual Reduction of Alcohol Intake: Instead of abruptly stopping alcohol consumption, gradually reducing alcohol intake over time can help prevent the onset of DTs. This method allows the body to adjust to lower levels of alcohol consumption and can be done with medical supervision.
- Treatment for Alcohol Use Disorder: Receiving treatment for alcohol use disorder can help reduce the chances of developing DTs in the future. Treatment approaches can include detoxification, cognitive behavioural therapy (CBT), recovery support groups, and various levels of care such as inpatient or outpatient programmes.
- Close Medical Supervision: Working closely with a healthcare provider can help manage alcohol withdrawal symptoms and prevent the onset of DTs. Doctors can prescribe medications such as benzodiazepines to treat alcohol withdrawal and prevent severe symptoms.
- Addressing Underlying Health Issues: DTs can be influenced by underlying health issues such as major injuries, liver or heart disease, traumatic brain injury, or psychiatric disorders. Addressing and managing these health conditions with a healthcare provider can be a preventative measure.
- Nutritional Support: Long-term alcohol misuse can lead to nutritional deficiencies, such as a lack of thiamine (vitamin B1). Ensuring a well-balanced diet or taking supplements under medical supervision can help prevent nutritional deficiencies associated with alcohol misuse.
- Early Intervention: Seeking early treatment for alcohol misuse can reduce the risk of developing DTs. The longer a person engages in heavy drinking, the higher the risk of experiencing DTs upon cessation. Therefore, addressing alcohol use disorder early on is a preventative measure.
Smart Devices to Monitor Alcohol Consumption at Home
You may want to see also

Long-term recovery
Delirium Tremens (DTs) is a severe and life-threatening form of alcohol withdrawal that requires immediate medical attention and often hospitalisation. DTs can be fatal and symptoms can worsen rapidly, so it is important to seek treatment as soon as possible.
Inpatient or residential care may be necessary for those with severe alcohol use disorder. Intensive outpatient programs (IOPs), partial hospitalization programs (PHPs), and outpatient care are also options for ongoing treatment. Sober living solutions, such as transitional housing or sober living homes, can provide a supportive environment for those in recovery.
Medications may also be prescribed to treat DTs and prevent symptom progression. Benzodiazepines are commonly used to treat alcohol withdrawal and DTs, as they help calm the nervous system. Antipsychotic drugs may also be administered to prevent hallucinations, a common symptom of DTs.
In addition to medical treatment, addressing underlying health issues and co-morbidities is crucial for long-term recovery. This includes managing any psychiatric disorders, such as depression, post-traumatic stress disorder, or bipolar disorder, which can increase the risk of developing DTs. Maintaining a well-balanced diet and addressing any nutritional deficiencies caused by long-term alcohol use can also support recovery.
Support from loved ones is also important during long-term recovery. Involving family members or caregivers in the treatment process can help them understand the condition and provide better support to their loved one. Additionally, support groups and recovery communities can offer ongoing encouragement and accountability during the recovery journey.
Storing Denatured Alcohol: Fire Cabinet Safe?
You may want to see also
Frequently asked questions
Symptoms of alcohol DTs include confusion, tremors, agitation, anxiety, psychosis, hallucinations, paranoia, disorientation, heavy sweating, seizures, irregular heart rate, and high blood pressure.
Alcohol DTs is a medical emergency and requires immediate treatment in a hospital. Call 911 or your local emergency number if you or someone you know has symptoms.
Treatment for alcohol DTs typically begins at the hospital, where the goal is to relieve symptoms, reduce the chance of complications, and save lives if necessary. Sedatives, such as benzodiazepines, are often used to calm the nervous system. If sedatives are ineffective, doctors may administer anesthesia to sedate the patient until symptoms subside. Intravenous fluids with vitamins and minerals may also be given to treat dehydration and restore electrolyte balance.