Alcoholic hepatitis is a potentially serious condition caused by alcohol misuse over a long period. Heavy drinking over years can damage the liver, and even shorter durations of alcohol abuse could lead to alcoholic hepatitis. Binge drinking, defined as consuming more than five drinks in a night for men or four for women, at least five times a month is considered heavy drinking. If this pace is kept up for as little as six months, the risk of developing alcoholic hepatitis rises significantly. However, it's important to note that not everyone who develops alcoholic hepatitis fits this profile, as some people are more sensitive to alcohol, and their livers react to even moderate use. The progression of liver disease is not solely dependent on the amount of alcohol consumed, and factors such as genetic differences and sex differences also play a role.
| Characteristics | Values |
|---|---|
| Possibility of developing alcoholic hepatitis in one year | Possible, but not common |
| Risk factors | Heavy drinking, genetic differences, family history of alcohol use disorder or liver disease, sex (men generally have a higher tolerance) |
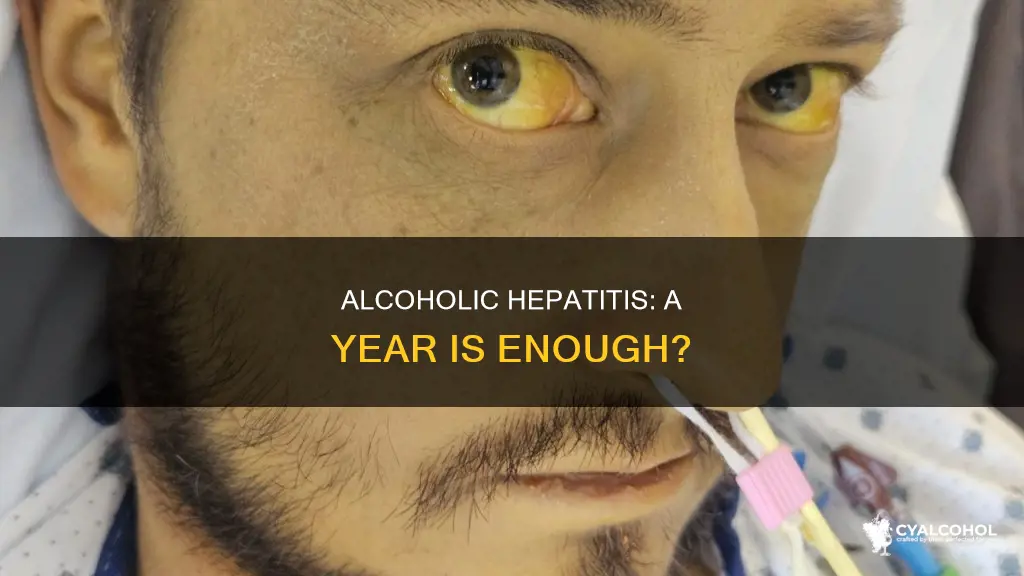
| Symptoms | Jaundice, fever, stomach ache, weight loss, liquid buildup in the belly, soreness in the upper right abdomen |
| Treatment | Stopping alcohol consumption, medications, therapy, support groups, diet changes, antibiotics, steroids, liver transplant in severe cases |
| Prevention | Reducing or stopping alcohol intake, sticking to recommended limits |
What You'll Learn

Heavy drinking and alcoholic hepatitis
Alcoholic hepatitis is inflammation of the liver caused by alcohol use. When alcohol is processed by the liver, it acts as a toxin, breaking down into poisonous chemicals. Chronic heavy drinking can overload the liver with fat and toxins, leading to alcoholic hepatitis. This condition is characterised by a history of chronic heavy alcohol consumption until at least 3 to 4 weeks before the onset of symptoms such as jaundice, fever, tachycardia, and tachypnea.
Heavy drinking is defined differently for men and women. For men, it involves consuming four or more standard drinks per day or more than 14 drinks per week. For women, it is defined as having three or more drinks per day or more than seven drinks per week. Binge drinking, which is consuming more than five drinks in a night for men or four for women, also falls under heavy drinking if it occurs at least five times a month.
The risk of developing alcoholic hepatitis rises significantly after maintaining this heavy drinking pace for as little as six months. However, most people diagnosed with alcoholic hepatitis have been drinking heavily for five years or more, with periods of abstinence. The progression of liver disease is not solely dependent on the duration and quantity of alcohol consumption, as some individuals develop alcoholic hepatitis from seemingly insignificant amounts of alcohol. Genetic differences and sex differences also play a role, with men generally being able to tolerate more alcohol than women.
If heavy drinking continues after a diagnosis of alcoholic hepatitis, the life expectancy rate decreases. For men who continue drinking heavily, the five-year survival rate is about 70%, while it drops to 30% for women. However, quitting alcohol after diagnosis can lead to significant improvement within six to 12 months, as the liver can heal some of its damage over time with complete alcohol avoidance.
In summary, heavy drinking can lead to alcoholic hepatitis, a serious condition causing inflammation of the liver. The risk of developing alcoholic hepatitis increases with prolonged heavy alcohol consumption, although individual factors such as genetics and sex also contribute to the progression of the disease. Quitting alcohol is crucial for improving prognosis and allowing the liver to recover from alcohol-induced damage.
Free Alcohol: Legal or Not in the UK?
You may want to see also

Risk factors and causes of alcoholic hepatitis
Alcoholic hepatitis is inflammation of the liver caused by alcohol use. It is not a viral condition and cannot be passed on to others. However, chronic heavy drinking can be considered "viral" in a social sense, as binge drinking with friends and family can reinforce the behaviour that leads to alcoholic hepatitis.
The risk of developing alcoholic hepatitis increases significantly after binge drinking at least five times a month for six months or more. Binge drinking is defined as consuming more than five drinks in a night for men or four for women. Heavy drinking over many years can damage the liver, but not everyone who develops alcoholic hepatitis fits this profile. Some people are more sensitive to alcohol, and their livers may react to even moderate alcohol consumption.
The amount of alcohol ingested is the most important risk factor for alcoholic hepatitis. However, the progression to alcohol-induced chronic liver disease is not solely dependent on the amount of alcohol consumed. Even shorter durations of alcohol abuse could lead to alcoholic hepatitis. A typical patient would be between 40 and 60 years old, with a history of consuming more than 100 g/day of alcohol for a decade.
Genetic differences may also play a role in susceptibility to alcoholic hepatitis. Individuals with a family history of alcohol use disorder or liver disease may be at a higher risk. Sex differences are also observed, with men generally tolerating more alcohol than women. However, it is important to note that there is no universally "safe" amount of alcohol consumption, as everyone's body is different.
Alcohol Cessation: Diarrhea a Common Withdrawal Symptom?
You may want to see also

Diagnosis and treatment options
Although it is unclear if it is possible to develop alcoholic hepatitis in one year, alcoholic hepatitis is typically characterized by a history of chronic heavy alcohol consumption. Even shorter durations of alcohol abuse could lead to alcoholic hepatitis.
Diagnosis
The diagnosis of alcoholic hepatitis is a clinical one with supporting laboratory findings. All patients should have an abdominal imaging study to exclude biliary obstruction and liver diseases such as liver cancer and liver abscess. Ultrasound is the first imaging test of choice to assess patients with alcoholic hepatitis; it can be used to exclude gallstones and other biliary tract disorders. A liver biopsy is not always required but is useful for excluding other disorders. Several trials and models exist to determine the severity of alcoholic hepatitis, to ascertain which patients would likely benefit from a pharmacological approach.
Typical laboratory findings in alcoholic liver disease include transaminase levels with aspartate aminotransferase greater than alanine aminotransferase, increased mean corpuscular volume, gamma-glutamyltranspeptidase, and IgA to IgG ratio. Carbohydrate-deficient transferrin is the most reliable marker of chronic alcoholism.
Treatment Options
Treatment options for alcoholic hepatitis include steroids, and in more severe cases, liver transplantation. A liver transplant may be considered for patients who are not responsive to steroids and have a MELD (Model for End-Stage Liver Disease) score of greater than 26. However, there are several barriers to liver transplantation, including fear of recidivism, organ shortage, and social and ethical considerations.
There are also helplines and support groups available for individuals and families facing alcohol-related issues, such as SAMHSA's National Helpline.
How Evaporation Transforms Alcohol: Chemistry or Physics?
You may want to see also

Reversing alcoholic hepatitis
Alcoholic hepatitis is a syndrome of jaundice and liver failure that occurs in heavy alcohol consumers. The diagnosis is usually based on a history of heavy alcohol consumption, blood tests, and the exclusion of other liver diseases. While heavy drinking over years can damage the liver, even shorter durations of alcohol abuse could lead to alcoholic hepatitis. Binge drinking, defined as more than five drinks in a night for men or four for women, at least five times a month, is considered heavy drinking.
If you have alcoholic hepatitis, the only way to reverse the damage and prevent further harm to your liver is to abstain from alcohol completely and forever. People who quit drinking alcohol after an alcoholic hepatitis diagnosis show great improvement after six to 12 months, with mild cases often resolving completely. However, it's important to note that existing scar tissue in the liver cannot be reversed. For severe cases of alcoholic hepatitis, treatment in a hospital may be necessary, and specific treatment with corticosteroids or pentoxifylline may be used to reduce liver inflammation.
Liver transplantation is a potential treatment for patients unresponsive to steroids, but it comes with its own set of challenges, including organ shortages and ethical considerations. Additionally, liver transplantation only provides short-term survival benefits, with no treatment currently increasing patient survival beyond three months.
It is important to note that stopping alcohol consumption is not easy, and many people with alcoholic hepatitis have alcohol dependency problems. Seeking psychological therapy, medication, and support groups like Alcoholics Anonymous can aid in abstaining from alcohol. Nutritional support is also crucial, as malnutrition is common in people with alcoholic liver disease.
Hot Garages: Bad Storage for Alcohol
You may want to see also

Liver transplantation considerations
While it is unclear if it is possible to develop alcoholic hepatitis in one year, several factors influence the progression of the disease. These include the amount and duration of alcohol consumption, age, sex, and genetic differences. Even shorter durations of alcohol abuse could lead to alcoholic hepatitis, and binge drinking at least five times a month is considered heavy drinking.
Liver transplantation is a viable option for patients with severe alcoholic hepatitis who do not respond to medical therapy. However, it is a controversial treatment option due to concerns about organ supply and the risk of patients resuming alcohol use after transplantation. The six-month rule, which requires patients to abstain from alcohol for six months before being considered for transplantation, has been a point of contention. While it aims to ensure patients' commitment to sobriety, it has been criticised for unfairly excluding otherwise suitable candidates.
The selection process for liver transplantation involves multiple criteria, including the severity of alcoholic hepatitis, the presence of supportive family members, the absence of severe coexisting or psychiatric disorders, and the patient's agreement to lifelong alcohol abstinence. Medical teams, addiction specialists, and hepatologists are involved in evaluating patients' suitability for transplantation.
The survival rates for patients who undergo liver transplantation for alcoholic hepatitis are promising, with comparable outcomes to patients with similar Model for End-Stage Liver Disease (MELD) scores. However, the risk of recidivism, or returning to alcohol use, remains a concern, and ethical considerations come into play when offering transplantation to patients with alcoholism.
Liver transplantation for alcoholic hepatitis is a complex decision that requires careful evaluation of each patient's circumstances and commitment to sobriety. While it offers improved survival rates, addressing alcohol use disorder is crucial to ensure long-term success and responsible utilisation of limited organ donations.
Alcoholism and Parenting: Navigating Disgust and Emotions
You may want to see also
Frequently asked questions
Yes, it is possible to develop alcoholic hepatitis in one year, especially if one engages in binge drinking, which is considered five or more standard drinks within a few hours for men and four for women, at least five times a month.
Risk factors for developing alcoholic hepatitis include heavy alcohol consumption over many years, genetic predisposition, and sex, with men generally being able to tolerate more alcohol than women.
Symptoms of alcoholic hepatitis can include jaundice, fever, stomachache, weight loss, and liquid buildup in the belly.
Alcoholic hepatitis is typically diagnosed through a combination of clinical evaluation and laboratory findings. Laboratory findings may include elevated liver enzymes, abnormal liver function tests, and imaging studies to exclude other liver diseases.
Treatment for alcoholic hepatitis focuses on addressing the underlying cause, which is alcohol misuse. The most critical part of treatment is complete and permanent abstinence from alcohol, which can lead to improvements within six to 12 months. Severe cases may require a liver transplant.