Alcoholism, or alcohol use disorder (AUD), is a complex condition influenced by a combination of genetic, physiological, psychological, and environmental factors. While there is no single alcoholic gene, research has identified specific genes associated with an increased risk of developing AUD. These genes can affect various biological processes and mental states, including physiological responses to alcohol, alcohol metabolism, addiction-related neurobiology, and behavioural tendencies such as impulsivity. For example, the genes ADH1B and ALDH2 have been found to have the largest effect on the risk for alcoholism, impacting alcohol metabolism and the body's response to it. Other genes, such as GABRA2 and GABRG1, have also been linked to alcohol dependence, with certain mutations increasing the risk of AUD. Genetic predispositions interact with environmental factors, such as childhood trauma, family history, and social influences, to contribute to the development of AUD. Understanding the interplay between genetics and environment is crucial for prevention, early intervention, and tailored treatment approaches for individuals struggling with alcohol misuse.
| Characteristics | Values |
|---|---|
| Alcoholism gene existence | Current evidence shows that certain genes associated with alcohol addiction can be inherited. |
| Genes associated with alcohol addiction | Alcohol dehydrogenase (ADH), aldehyde dehydrogenase (ALDH), CHNR5, GCKR, DRD2, GABRA2, GABRG1, Beta-Klotho, GABRB1 |
| Gene impact | Affecting tolerance, the central nervous system's response to alcohol, alcohol metabolism, addiction-related neurobiology, behavioural tendencies, and more. |
| Gene prevalence | ADH1B is prevalent in 70% of East Asians, but has a low prevalence in European populations. |
| Genetic testing | There are no specific alcoholism genetic tests, but standard diagnostic tests for AUD exist. |
| Genetic predisposition | Genes can increase the risk of developing an addiction, but do not guarantee an alcohol use disorder. |
| Environmental factors | Family history, childhood abuse, parental struggles, mental illness, and stress are environmental factors that contribute to the risk of developing an addiction. |
| Preventative measures | Education, alcohol-free activities, family rules, skill-building, and youth leadership programs can help prevent or delay alcohol use in children. |
What You'll Learn

Alcoholism gene: fact or fiction?
It is a fact that certain genes are associated with alcohol addiction and can be inherited. However, having the "alcoholism gene" does not guarantee that a person will develop an alcohol use disorder (AUD). Instead, it means that they have a risk factor that, when combined with other risk factors, increases their likelihood of experiencing alcohol-related issues.
Genes associated with the risk for alcoholism include alcohol dehydrogenase 1B (ADH1B) and aldehyde dehydrogenase 2 (ALDH2). These genes are central to the metabolism of alcohol, primarily in the liver. Other genes that have been linked to an increased risk of AUD include CHNR5, GCKR, and DRD2. These genes are involved in how the central nervous system responds to alcohol.
Research has also identified several other genes that contribute to the risk of alcohol dependence and key endophenotypes. For example, a group of SNPs within the GABRA2 gene has been associated with alcohol dependence, particularly in individuals with early-onset or comorbid drug dependence. Additionally, mutations in the GABRB1 gene can increase the risk of AUD by altering the availability of gamma-aminobutyric acid (GABA) in the brain, which influences relaxation and stress relief.
It is important to note that gene expression is influenced by environmental factors. Childhood abuse, parental struggles, mental illness in the family, and exposure to trauma or stressors can all contribute to the development of AUD. Therefore, while genetics play a significant role in AUD risk, it is not the sole determinant.
Currently, there are no specific genetic tests for alcoholism. However, researchers are making significant progress in understanding the genetic basis of AUD, which may lead to future developments in genetic testing and more targeted treatment or prevention strategies.
Cleaning Glasses with Alcohol: Safe or Not?
You may want to see also

Genes and their impact on alcohol metabolism
Alcoholism, or alcohol dependence, is a complex disorder influenced by various factors, including genetics and environmental factors. While there is no single "alcoholic gene," certain genes have been identified that contribute to the risk of developing alcohol use disorder (AUD). These genes are involved in how an individual's body metabolises alcohol, and their impact on the central nervous system's response to it.
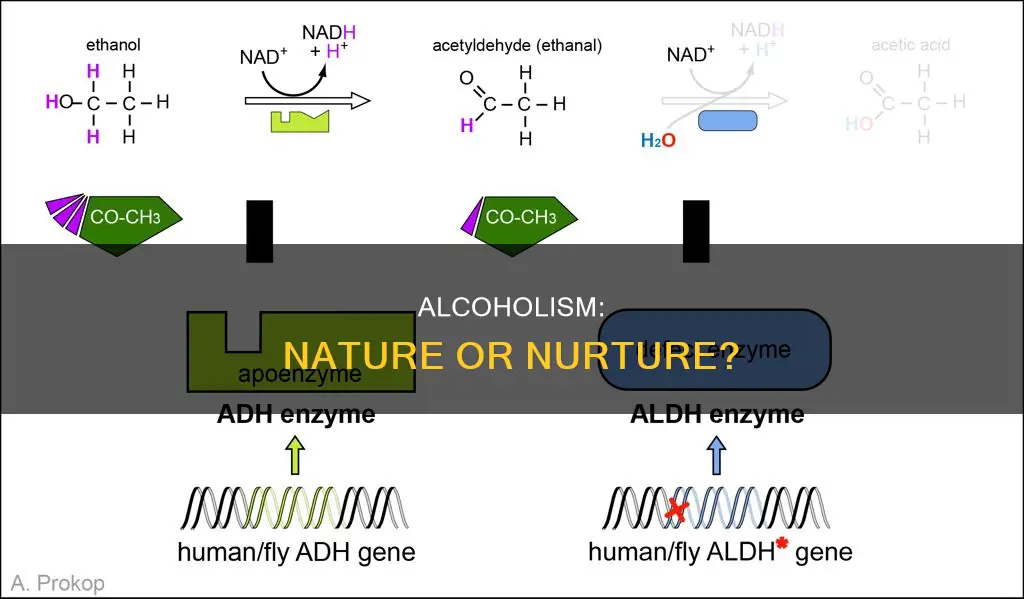
Gene variants encoding several alcohol-metabolising enzymes, such as alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH), are among the most significant genetic associations with the risk for alcohol dependence. These enzymes play a crucial role in breaking down alcohol (ethanol) in the body, primarily in the liver. The ADH enzymes catalyse the first step of ethanol metabolism, converting it into acetaldehyde, while ALDH enzymes facilitate the second step, metabolising acetaldehyde into acetate.
Acetaldehyde is a toxic intermediate product, and its accumulation can lead to unpleasant symptoms such as dizziness, nausea, and increased heart rate (tachycardia). Certain genetic variants, or alleles, of the ADH and ALDH genes have been associated with lower rates of alcohol dependence. For example, the ADH1B*2, ADH1B*3, ADH1C*1, and ALDH2*2 alleles are linked to reduced alcohol dependence. These alleles are differentially distributed among ethnic groups, with ADH1B*2 found frequently in Northeast Asians and occasionally in Caucasians, ADH1B*3 predominantly in individuals of African ancestry, and ALDH2*2 almost exclusively in Northeast Asians.
The presence of specific alleles can influence the rate at which alcohol or acetaldehyde is metabolised, thereby affecting an individual's response to alcohol and their drinking behaviour. For instance, certain alleles of the ADH1B and ADH1C genes encode highly active ADH enzymes, leading to a more rapid conversion of ethanol to acetaldehyde. These alleles have a protective effect against alcoholism. On the other hand, slower metabolism of acetaldehyde due to certain ALDH alleles can result in higher acetaldehyde levels, causing unpleasant reactions and potentially increasing the risk of alcohol dependence.
In addition to ADH and ALDH genes, other genes have been implicated in the risk for alcohol dependence. These include the GABRA2 gene, which has been associated with alcohol dependence, particularly in individuals with early onset or comorbid drug dependence. The COGA investigators also explored the potential involvement of the adjacent GABRG1 gene. Furthermore, the beta-Klotho gene has been linked to lower alcohol consumption, as individuals with this gene tend to consume fewer drinks and exhibit better control over their drinking behaviour.
While genetics play a significant role in the development of AUD, it is essential to understand that it is just one piece of the puzzle. Environmental factors, such as childhood trauma, parental substance abuse, mental illness in the family, and socioeconomic stressors, also contribute significantly to the risk of AUD. The interplay between genetic predispositions and environmental influences shapes an individual's relationship with alcohol and their risk of developing alcohol dependence.
Illinois Alcohol Sales: What's the Latest Update?
You may want to see also

The influence of environment on genetic predispositions
While there is a genetic component to alcohol use disorder (AUD), it is not the sole factor. Gene variants such as alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) are associated with how the body metabolises alcohol, which may be inherited. However, the environment in which a person is raised also contributes significantly to the development of AUD.
Childhood abuse, parental struggles, mental illness in the family, and exposure to trauma or stress are environmental factors that can increase the risk of AUD. These factors can influence a person's stress response and mental health, which are also risk factors for AUD. The interplay between genetic predispositions and these environmental factors can create a higher risk for AUD.
For example, individuals with certain genetic variants may experience an alcohol flush reaction, causing them to feel hot, sweaty, and sick when consuming alcohol. This reaction serves as a deterrent to alcohol use. However, in populations with a lower frequency of this gene variant, such as Europeans, there may be an increased risk of AUD due to fewer genetic deterrents. Similarly, the beta-Klotho gene is associated with drinking less and better controlling alcohol consumption. People without this gene may have a higher risk of AUD due to their inability to regulate their drinking.
Additionally, family history and genetics are closely linked, and specific genes associated with AUD can be inherited. Studies have found that family members pass down multiple genes that are risk factors for developing an addiction. For instance, the ADH1B gene has a low prevalence in European populations but is prevalent in 70% of East Asians. Thus, environmental factors, such as cultural and geographical differences, can influence the prevalence of certain genes and subsequently impact the risk of AUD.
Furthermore, the development of AUD can be influenced by the interaction of genetic and environmental factors. For instance, individuals with mental illnesses, particularly anxiety, depression, bipolar disorder, and schizophrenia, are more likely to struggle with co-occurring AUD. The presence of these mental illnesses, which can be influenced by environmental factors, can increase the risk of AUD.
In summary, while there may be a genetic predisposition to AUD, it is essential to consider the influence of environmental factors. The interplay between genetics and environment contributes to the development of AUD, and addressing both aspects is crucial for understanding and managing alcohol-related disorders.
Alcohol Package on Royal Caribbean: Worth the Money?
You may want to see also

Alcohol tolerance and its inheritability
Alcohol tolerance refers to the body's ability to suppress normal responses to alcohol. It is a prominent symptom of alcohol addiction and is influenced by the body's alcohol metabolism. Alcohol tolerance is increased by regular drinking, and people with high alcohol tolerance are more likely to engage in binge drinking.
Genetics plays a significant role in alcohol tolerance, with certain genes affecting alcohol metabolism and influencing tolerance levels. For example, the genes with the clearest contribution to the risk for alcoholism and alcohol consumption are alcohol dehydrogenase 1B (ADH1B) and aldehyde dehydrogenase 2 (ALDH2). These genes are central to the metabolism of alcohol, with ADH enzymes catalysing the oxidation of ethanol to acetaldehyde and ALDH enzymes metabolising acetaldehyde to acetate. Higher body masses and the prevalence of high levels of alcohol dehydrogenase in an individual increase alcohol tolerance, and both adult weight and enzymes vary with ethnicity.
However, not all differences in tolerance can be traced to biochemistry. Differences in tolerance levels are also influenced by socio-economic and cultural differences, including diet, average body weight, and patterns of consumption. Additionally, while genetic risk is about half of the problem, family history accounts for the other half. People with a family history of alcoholism may develop a tolerance that causes them to drink more to feel the same effects. This is known as acute tolerance to alcohol.
Furthermore, gene expression is affected by the environment. If a person grows up in a household with a parent who abuses drugs, struggles with mental illness, or experiences significant stress, and the child has a gene linked to alcohol use disorder, their risk of developing an alcohol addiction increases.
While specific genes associated with alcohol addiction can be inherited, having the alcoholism gene does not guarantee an alcohol use disorder.
David's Drinking: Exploring Alcoholism in My Lottery Dream Home
You may want to see also

The link between mental health and alcoholism
Alcoholism, or alcohol use disorder (AUD), is a complex condition influenced by a combination of genetic, physiological, psychological, and environmental factors. While there is no single "alcoholic gene," research has identified specific genes associated with an increased risk of developing AUD and related mental health issues.
Genetics play a significant role in the development of AUD, with studies suggesting that 40% to 60% of the vulnerability to AUD is inherited. Certain gene variants, such as alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH), are involved in alcohol metabolism and can affect an individual's tolerance to alcohol. For example, the ADH1B gene, which is prevalent in East Asians, has been linked to increased risk. Additionally, genes like GABRA2 and GABRG1 have been associated with alcohol dependence, particularly in individuals with early onset or comorbid drug dependence.
The interplay between genetic factors and environmental influences can further increase the risk of AUD. Individuals with a family history of alcohol misuse, childhood trauma, or exposure to significant stressors are more susceptible to developing AUD. Mental health conditions, such as anxiety, depression, bipolar disorder, and schizophrenia, often co-occur with AUD, creating a complex interplay between genetic predispositions and environmental triggers.
It is important to note that having these genes does not guarantee the development of AUD. Gene expression is influenced by environmental factors, and not all individuals with the associated genes will develop an alcohol use disorder. However, understanding the genetic contributions to AUD can help guide prevention, early intervention, and personalized treatment approaches.
To assess the risk of AUD, healthcare professionals utilize diagnostic tools such as the Alcohol Use Disorders Identification Test (AUDIT) and its shorter version, AUDIT-C. These screening tools evaluate alcohol consumption patterns, drinking behaviours, and potential dependence to determine the likelihood of AUD.
Carnival Cruise Alcohol Package: Worth the Money?
You may want to see also
Frequently asked questions
Yes, certain genes are associated with alcohol addiction and can be inherited. However, having the gene does not guarantee an alcohol use disorder (AUD).
Genes associated with an increased risk of AUD include alcohol dehydrogenase (ADH), aldehyde dehydrogenase (ALDH), CHNR5, GCKR, and DRD2.
Genes can impact the body's metabolism of alcohol, the central nervous system's response to alcohol, and behavioural tendencies such as impulsivity. For example, individuals with an innate alcohol tolerance may be at increased risk of heavy drinking and AUD.
Genetics and family history are the most correlated with the risk of AUD. About 40% to 60% of people with AUD have genes that increase their risk of developing an addiction.
While there are no specific genetic tests for alcoholism, there are standard diagnostic tests for AUD, such as the Alcohol Use Disorders Identification Test (AUDIT) and its shorter version, AUDIT-C. These tests assess alcohol consumption, drinking behaviours, and alcohol-related problems.