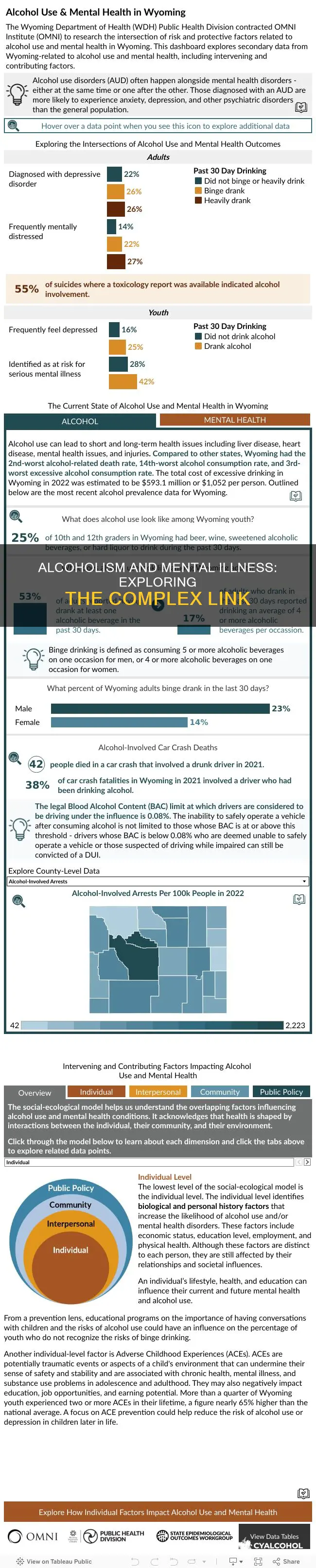
Alcoholism and mental illness are closely intertwined. Alcohol is a depressant that disrupts the balance of neurotransmitters in the brain, affecting feelings, thoughts, and behavior. It can lead to psychological disturbances and is recognized as a disease by organizations like the American Medical Association (AMA). Alcohol use disorder (AUD) frequently co-occurs with mental health disorders, and individuals may use alcohol to self-medicate or cope with symptoms of mental illness. Conversely, alcohol misuse can intensify symptoms of mental health conditions, and the two conditions can influence each other in a vicious cycle. The relationship between alcohol and mental health is complex, and understanding this link is crucial for accurate diagnosis and effective treatment.
| Characteristics | Values |
|---|---|
| Alcohol use disorder (AUD) and mental health disorders | Co-occur frequently |
| Reasons for co-occurrence | Self-medication, genetic, biological, environmental, and social factors |
| Mental health disorders that co-occur with AUD | Depression, bipolar disorder, anxiety, PTSD, schizophrenia |
| AUD treatment | Severity of AUD and co-occurring disorder determines the level of care |
| Alcohol as a depressant | Disrupts balance of neurotransmitters in the brain, affecting feelings, thoughts, and behavior |
| Alcohol and impulsivity | Alcohol lowers inhibitions, leading to impulsive actions such as self-harm or suicide |
| Alcohol and mental health problems | Alcohol misuse can lead to or worsen mental health issues, and vice versa |
| Alcohol and the brain's reward center | Alcohol affects dopamine levels, leading to compulsive decision-making and impulsive behavior |
| Diagnostic challenges | Alcohol-related symptoms can complicate or mimic psychiatric syndromes, making accurate diagnosis difficult |
What You'll Learn

Alcohol use disorder (AUD) and depression
Depression is a mood disorder characterized by persistent feelings of sadness, numbness, or irritability, accompanied by cognitive and physical symptoms such as worthlessness, difficulty concentrating, fatigue, and lack of energy. Individuals experiencing depressive symptoms may turn to alcohol as a form of self-medication to alleviate their symptoms and feel better. However, this can lead to the development of AUD. The co-occurrence of AUD and depression is associated with greater severity and a worse prognosis for both disorders.
Research suggests that alcohol can not only trigger depressive symptoms but also exacerbate existing ones. A study in JAMA Psychiatry found a potential cause-and-effect relationship between alcohol misuse and major depressive disorder. Additionally, individuals with a genetic predisposition to depressive disorders may be more susceptible to the depressive effects of alcohol. Depressive symptoms caused by alcohol often improve significantly after abstaining from alcohol for a period, typically around 3-4 weeks. However, it is important to note that substance-induced depression can sometimes persist even after discontinuing alcohol, transforming into independent depression.
The link between AUD and depression is bidirectional, with each condition influencing the other. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) reports that the lifetime prevalence of co-occurring depression and AUD is 27% to 40%, while the 12-month prevalence is up to 22%. This highlights the significant overlap between these disorders. Treatment for co-occurring AUD and depression often involves an integrated approach, addressing both conditions simultaneously. However, the severity of AUD and depression determines the level of care required, with more severe cases necessitating specialized mental health and addiction services.
It is crucial to seek professional help when dealing with AUD and depression. Healthcare professionals can provide guidance, support, and tailored treatment plans to address these co-occurring disorders effectively.
Alcoholism and Verbal Abuse: A Common Combination?
You may want to see also

Self-medication and mental illness
Alcohol use disorder (AUD) and mental health disorders often co-occur. People experiencing symptoms of a mental health condition may attempt to self-medicate with alcohol. Self-medication refers to the purposeful act of individuals with mental disorders perceiving their symptoms as treatable and using substances to mitigate them.
Alcohol is a depressant that can disrupt the balance of neurotransmitters in the brain, affecting feelings, thoughts, and behaviour. It can make a person feel relaxed, less anxious, and more confident, but these effects are temporary. As alcohol wears off, one often feels worse due to its withdrawal effects on the brain and body.
People drink for various reasons, including to celebrate, socialize, commiserate, or cope with depression, stress, anxiety, or other difficult feelings. However, drinking heavily or using drugs to self-medicate can lead to the development of new mental health problems. For example, opioid and alcohol use have been linked to triggering depression, while marijuana and methamphetamine use have been associated with psychosis.
Self-medication can also worsen existing symptoms or generate new ones, interact negatively with prescription medications, and cause problems in one's life and relationships. It can also delay or prevent individuals from seeking professional help for their mental health issues.
If you are struggling with self-medication or substance abuse, it is important to recognize when and how you are self-medicating and seek help from a healthcare professional. There are healthier and more effective ways to cope with mental health issues and manage your emotions.
Propylene Glycol vs Cetostearyl Alcohol: What's the Difference?
You may want to see also

Alcoholism and suicidal thoughts/attempts
Alcohol use disorder (AUD) and mental health disorders are closely linked. Mental health conditions that commonly co-occur with AUD include depression, bipolar disorder, anxiety, PTSD, and schizophrenia.
Alcohol acts as a depressant in the body, disrupting the balance of neurotransmitters (chemical messengers) in the brain and affecting feelings, thoughts, and behavior. While alcohol may initially make someone feel relaxed, less anxious, and more confident, these effects quickly wear off, and can be replaced by negative feelings such as anger, depression, or anxiety. Alcohol also slows down how the brain processes information, making it harder to identify true feelings and the possible consequences of one's actions. This can lead to actions such as self-harm or suicide.
Heavy drinking is linked to suicidal thoughts and attempts. A state of intoxication may trigger self-inflicted injuries by increasing impulsivity, promoting depressive thoughts and feelings of hopelessness, and removing inhibiting barriers to self-harm. Alcohol abuse may lead to suicidality through disinhibition, impulsiveness, and impaired judgment. It is important to note that alcohol consumption can also be a form of self-medication for underlying depression or other high-risk behaviors.
People with depression should be screened for suicide risk by being asked specifically about suicidal thoughts and plans. If suicidal ideation is present or suspected, risk factors for suicide should be assessed. If suicide risk is present, further assessment should address the imminence of suicidal behavior. Intention to die, cogent plans, and high levels of hopelessness might indicate imminent risk.
Universal preventive interventions are directed at the entire population, while selective interventions target people at greater risk for suicidal behavior, such as those with psychiatric disorders, alcohol and/or drug abuse, newly diagnosed severe physical illness, past suicide attempts, homelessness, institutionalization, and other types of social exclusion.
Furnishing Alcohol to Minors: Felony in Pennsylvania?
You may want to see also

Alcoholism as a mental illness
Alcoholism, or alcohol use disorder (AUD), is closely linked to mental illness. Alcohol is a depressant that affects the brain's reward centre by disrupting the balance of neurotransmitters, our brain's "feel-good" chemicals. When the brain experiences a flood of dopamine-induced pleasure, it learns to seek drugs or alcohol at the expense of healthier goals and activities. This can lead to compulsive decision-making, impulsive behaviour, and relapse, which are characteristic of addiction.
Alcoholism and mental illness often co-occur, with alcohol acting as a form of self-medication for those experiencing mental health issues. Mental health conditions that commonly co-occur with AUD include depression, bipolar disorder, anxiety, PTSD, and schizophrenia. For example, a person with PTSD may develop AUD as a result of using alcohol to cope with or numb traumatic memories. Similarly, people with depression may drink alcohol to feel more relaxed, courageous, or confident. However, as the effects of alcohol wear off, individuals often experience a worsening of symptoms, known as alcohol withdrawal.
The relationship between alcoholism and mental illness is complex and bidirectional. Alcohol misuse can lead to the development or exacerbation of mental health problems, while pre-existing mental health disorders can increase the risk of alcohol misuse. This bidirectional relationship can create diagnostic challenges for clinicians, who must differentiate between alcohol-related symptoms and independent psychiatric disorders. Heavy alcohol use can also impair memory, further complicating the diagnostic process.
Treating alcoholism and co-occurring mental illness requires a comprehensive and integrated approach. Depending on the severity of AUD and mental health conditions, individuals may receive treatment from primary care providers, mental health specialists, addiction specialists, or a combination of these professionals. Addressing both alcoholism and mental health disorders simultaneously can improve treatment outcomes and reduce illness severity. Recovery is possible, particularly when both conditions are treated concurrently by licensed professionals.
Overall, the link between alcoholism and mental illness is well-established, and the two conditions often coexist and influence each other. Effective treatment requires a nuanced understanding of this complex relationship and a tailored approach that addresses the specific needs of each individual.
Alcoholism: Illness or Personality Trait?
You may want to see also

Genetic links between AUD and mental illness
While there is no specific gene that directly causes Alcohol Use Disorder (AUD), abundant evidence indicates that alcoholism is a complex genetic disease. Gene variants such as alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) are associated with how the body metabolises alcohol and may be inherited. For example, the ADH1B gene is very prevalent in East Asians, with 70% of the population possessing it. This gene is associated with the alcohol flush reaction, which can cause an increase in feelings of sickness and discomfort. Populations with a lower frequency of this gene, such as Europeans, have an increased risk of developing AUD due to fewer genetic deterrents.
The National Institute on Drug Abuse reported on a study of over 1 million people, which found that family members pass down multiple genes that are risk factors for developing an addiction. Researchers identified several genes that are candidates for being inheritable addiction genes, including ADH1B, CHNR5, GCKR, and DRD2. These genes are involved in how the central nervous system responds to alcohol and how the body metabolises it.
Family, twin, and adoption studies have further confirmed the genetic component of alcoholism. A study in Sweden followed alcohol use in twins who were adopted as children and raised apart. The incidence of alcoholism was significantly higher among twins whose biological fathers were alcoholics, regardless of the presence of alcoholism in their adoptive families.
In addition to genetics, environmental factors also play a crucial role in the development of AUD. Childhood trauma, parental influence, and living with mental illness can increase the risk of AUD. Living in an unhealthy or stressful environment can negatively impact drinking habits and decisions. The interplay between genetic and environmental factors can also contribute to the development of mental health conditions such as anxiety and depression, which further raise the risk of AUD.
While genetics may predispose individuals to developing AUD, it is not the sole cause. Prevention and education programs, as well as appropriate therapy to manage mental and behavioural conditions, can help address this risk.
Pothead vs Alcoholic: Is There a Difference?
You may want to see also
Frequently asked questions
Yes, alcohol problems and mental ill health are closely linked. Research shows that people who drink alcohol are more likely to develop mental health problems, and people with severe mental illness are more likely to have alcohol problems.
People may drink to try to relieve the symptoms of mental ill health. Alcohol acts as a depressant in the body, but it may lower a person's inhibitions and seem like a stimulant at first. This can make people feel more relaxed, courageous, or confident. However, the effect of alcohol is only temporary, and as it wears off, people often feel worse.
Alcohol misuse can lead to psychological disturbances and intensify the symptoms of mental illness. Heavy drinking is also linked to suicidal thoughts and attempts.
Treatment can be more complicated when a person suffers from co-occurring alcoholism and mental illness. Depending on the person's circumstances, healthcare professionals may prioritize treating either alcoholism or the mental illness first, or they may opt for a treatment plan that addresses both simultaneously.
Research shows that individuals who are susceptible to addiction or genetically predisposed to certain mental health disorders likely have lower levels of dopamine in their brains. When the brain's reward centers are flooded with alcohol-induced dopamine, the brain learns to seek drugs or alcohol instead of healthier goals and activities.