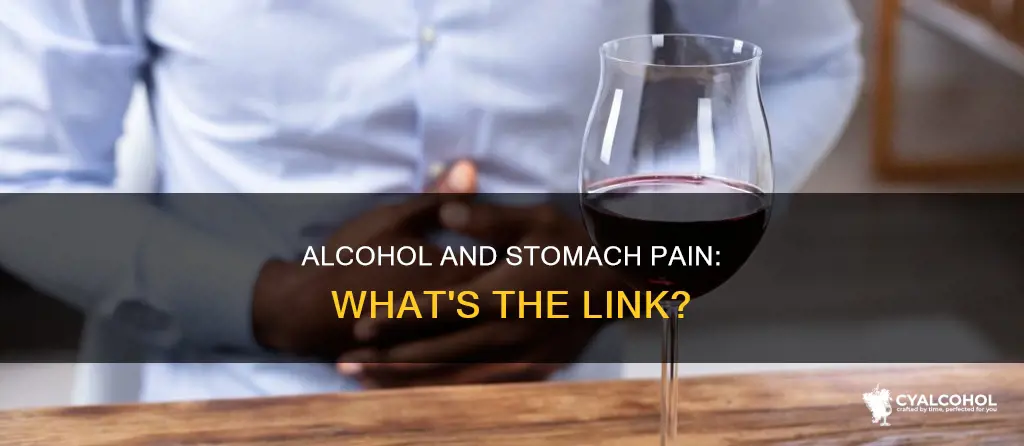
Alcoholic beverages can irritate the stomach and cause a burning sensation. This is known as alcoholic gastritis, which is caused by drinking too much, too often. The alcohol irritates and erodes the stomach lining, causing inflammation and pain. This can lead to the development of painful ulcers in the stomach lining. Alcohol intolerance, a genetic condition affecting the body's ability to digest alcohol, can also cause a burning sensation in the stomach. Other symptoms of alcohol intolerance include itching skin, redness, warmth in the skin, nasal congestion, a runny nose, asthma, headaches, an increased heart rate, vomiting, cramping, abdominal pain, and nausea.
| Characteristics | Values |
|---|---|
| Burning sensation in the stomach | Alcohol intolerance, allergy, or irritation/inflammation from histamine production |
| Cause of burning sensation | Alcohol remaining undigested and aggravating the stomach and intestine linings |
| Other symptoms | Itching skin, redness, warmth in the skin, nasal congestion, runny nose, asthma, headaches, increased heart rate, vomiting, cramping, abdominal pain, nausea |
| Effects of drinking alcohol | Acid reflux, heartburn, gastritis, stomach ulcers, increased risk of certain cancers |
| Recommendations | Drink less alcohol, follow low-risk drinking guidelines, avoid binge drinking, drink water or soft drinks in between alcoholic drinks |

Alcohol intolerance
It is important to distinguish alcohol intolerance from an alcohol allergy. While alcohol intolerance is a digestive system disorder, an alcohol allergy is an immune system response to ingredients in alcoholic beverages, such as grains, chemicals, or preservatives. Allergic reactions to alcohol can cause symptoms similar to alcohol intolerance, including difficulty breathing, coughing, a runny nose, or stomach upset. However, these symptoms may be triggered by even a small sip of alcohol.
While it is not normal for alcohol to cause a burning sensation in the stomach, drinking alcohol is associated with acid reflux or heartburn. Alcohol can cause the stomach to produce more acid than usual, leading to inflammation and pain (gastritis). Over time, this can result in the development of painful stomach ulcers, which alcohol can also worsen or slow the healing process for. Therefore, it is important to drink within the recommended guidelines and avoid binge drinking to minimize the negative effects of alcohol on the stomach.
Alcohol Distillation: Legal in Washington State?
You may want to see also

Acid reflux
Drinking alcohol is associated with acid rising from the stomach into the throat, known as acid reflux, which can cause heartburn. Alcohol consumption can make the stomach produce more acid than usual, which can wear away the stomach lining and cause inflammation and pain (gastritis). Over time, this can lead to the development of painful stomach ulcers.
Alcohol can also affect the tissues in the stomach, making them more sensitive to acid, which can, in turn, lead to heartburn. This is a painful, burning sensation in the chest and upper throat, caused by stomach acid flowing back into the oesophagus. This condition is known as gastroesophageal reflux disease (GERD), which is characterised by the abnormal reflux of gastric contents into the oesophagus.
GERD has two forms: reflux oesophagitis (RE) and non-erosive reflux disease (NERD). The symptoms of GERD are chronic and can significantly impair an individual's quality of life. Exposure of the oesophagus and stomach to alcohol can cause direct damage to the mucosal tissues in these organs. Additionally, the toxic acetaldehyde metabolised from alcohol could affect the function of the oesophagus and stomach.
To reduce the risk of negative effects on the stomach, it is recommended to limit alcohol consumption to low-risk drinking guidelines, which advise not drinking more than 14 units of alcohol per week and avoiding binge drinking. Drinking water or soft drinks in between alcoholic beverages can also help reduce overall alcohol consumption.
Cold or Warm: Which is the Best Way to Store Alcohol?
You may want to see also

Gastritis
The symptoms of gastritis vary among individuals but may include stomach upset or pain, belching and hiccups, nausea and vomiting, a feeling of fullness or burning in the stomach, and loss of appetite. In more severe cases, there may be blood in the vomit or black stool, indicating possible bleeding in the stomach.
Alcohol consumption is a common cause of gastritis. It can lead to acid reflux, where stomach acid rises into the throat, causing heartburn. Alcohol can also increase acid production in the stomach, gradually eroding the stomach lining and causing inflammation and pain. This can eventually lead to the development of painful ulcers in the stomach lining. Acute gastritis can occur after a single session of heavy drinking, while chronic gastritis develops over more extended periods of alcohol consumption.
To diagnose gastritis, healthcare providers may perform an upper GI (gastrointestinal) series or barium swallow X-ray to examine the upper digestive system. They may also collect stool and breath samples to test for the presence of H. pylori bacteria, a common cause of gastritis. Treatment for gastritis depends on the underlying cause and may include antibiotics, antacids, and other medications to reduce stomach acid and promote healing.
To prevent alcohol-related gastritis, it is important to follow low-risk drinking guidelines, avoid binge drinking, and have several drink-free days per week. Drinking water or soft drinks between alcoholic beverages can also help reduce the overall amount of alcohol consumed.
Shipping Alcohol: What's the Legal Status?
You may want to see also

Stomach ulcers
Alcohol is known to cause a burning sensation in the stomach, which is often referred to as heartburn or acid reflux. This occurs when acid rises from the stomach into the throat. Drinking alcohol can cause the stomach to produce more acid than usual, which can, over time, erode the stomach lining, causing inflammation and pain known as gastritis.
Gastritis can increase the risk of developing stomach ulcers, which are painful open sores in the stomach lining. Ulcers can cause nausea and vomiting, and alcohol can exacerbate these symptoms and slow down the healing process. In addition to avoiding alcohol, those with ulcers may be advised to stay away from spicy foods, acidic beverages, smoking, caffeine, and certain medications.
Drinking alcohol is also associated with an increased risk of several cancers, including those of the mouth, upper throat, food pipe, bowel, and liver. To reduce the risk of negative effects on the stomach, it is recommended to follow low-risk drinking guidelines, which advise against regular drinking of more than 14 units of alcohol per week and binge drinking. Drinking water or soft drinks in between alcoholic beverages can also help reduce overall alcohol consumption.
If you are experiencing any symptoms or discomfort, it is always best to consult a doctor or healthcare professional for personalized advice and treatment. They may suggest dietary changes, lifestyle modifications, or medications to help manage your condition.
Red Nose and Alcoholism: Is There a Link?
You may want to see also

Nutritional deficiencies
Alcoholic beverages can cause a burning sensation in the stomach and lead to several nutritional deficiencies. Alcohol can cause acid reflux, where acid rises from the stomach into the throat, resulting in heartburn. This occurs when the stomach produces more acid than usual, which can wear away the stomach lining, causing inflammation and pain known as gastritis. Heavy drinking can also impair the body's ability to absorb vital nutrients, particularly proteins, vitamins, and minerals. As a result, regular heavy drinkers are likely to become deficient in several nutrients.
Alcoholic gastritis is a condition characterised by inflammation and irritation of the stomach lining due to excessive alcohol consumption or alcohol addiction. The chronic presence of alcohol can erode the stomach's protective layer, leading to various uncomfortable and painful symptoms, including abdominal pain, indigestion, fatigue, and heartburn. Untreated alcoholic gastritis can lead to severe complications, including internal bleeding.
To prevent nutritional deficiencies caused by alcohol-related stomach issues, it is crucial to reduce alcohol consumption. Drinking less alcohol overall, alternating alcoholic beverages with water or soft drinks, and following low-risk drinking guidelines can help minimise negative effects on the stomach. Additionally, avoiding binge drinking and having several drink-free days per week are important for maintaining digestive health and nutrient absorption.
In summary, alcohol can cause a burning sensation in the stomach due to acid reflux and gastritis, leading to nutritional deficiencies. Alcoholic gastritis impairs nutrient absorption and can result in malnutrition. To prevent nutritional deficiencies, it is essential to reduce alcohol consumption, follow healthy drinking practices, and seek medical attention for stomach-related issues.
Alcohol Dependence: Whose Problem Is It Anyway?
You may want to see also
Frequently asked questions
It is not uncommon for alcohol to cause a burning sensation in your stomach. This could be a sign of alcohol intolerance, which is caused by a genetic condition that affects your body's ability to digest alcohol. Other causes could be acid reflux, inflammation, or gastritis. If you are experiencing these symptoms, it is best to consult a medical professional.
Alcohol intolerance is often referred to as an alcohol allergy due to its allergy-like symptoms. It is caused by a lack of enzymes in the small intestines needed to break down alcohol, leaving it undigested and allowing it to irritate the stomach lining. This condition has no cure, and the only way to prevent symptoms is to eliminate alcohol from your diet.
Aside from a burning stomach, symptoms of alcohol intolerance include itching skin, redness, warmth in the skin, nasal congestion, a runny nose, asthma, headaches, an increased heart rate, vomiting, cramping, abdominal pain, and nausea. These symptoms can develop within minutes of consuming alcohol and can be severe.
To reduce the risk of negative effects on your stomach, it is recommended to lower your overall alcohol intake. You can do this by alternating alcoholic drinks with water or soft drinks, or by choosing non-alcoholic alternatives. Following your local low-risk drinking guidelines and avoiding binge drinking can also help.